WASHINGTON (AP) — President Joe Biden's administration on Tuesday announced new rules meant to push insurance companies to increase their coverage of mental health treatments.
The new regulations, which still need to go through a public comment period, would require insurers to study whether their customers have equal access to medical and mental health benefits and to take remedial action, if necessary. The Mental Health Parity and Addiction Equity Act requires that insurers provide the same level of coverage for both mental and physical health care — though the administration and advocates argue insurers' policies restrict patient access.
The rules, if finalized, would force insurers to study patient outcomes to ensure the benefits are administered equally, taking into account their provider network and reimbursement rates and whether prior authorization is required for care.
“Too many Americans still struggle to find and afford the care they need,” the White House said in an emailed statement.
The Democratic president's administration said it's aiming to address issues such as insurers enabling nutritional counseling for diabetes patients but making it more difficult for those with eating disorders.
By measuring outcomes, the White House said, it will force insurers to make modifications to come into compliance with the law.
The U.S. Treasury Department has changed the standard for what kind of electric vehicles qualify for a federal tax benefit under the Inflation Reduction Act.
New York Republican Rep. George Santos is temporarily stepping down from his congressional committee assignments amid ongoing investigations surrounding his fabrications.
British energy giant BP predicts that fossil fuels as a primary energy source will decline from 80 percent in 2019 to between 55 and 20 percent in 2050.
The costs of COVID-19 vaccines are expected to skyrocket once the government stops buying them, with Pfizer saying it will charge as much as $130 per dose, and millions of people are expected to be kicked off of Medicaid.
TikTok CEO Shou Zi Chew will testify before Congress in March about the app's security and its ties to China.
The House Speaker said he wants to address spending cuts along with raising the debt limit, even though the White House has ruled out linking those two issues together as the government tries to avoid a potentially devastating financial default.
The Federal Reserve's preferred gauge of inflation showed the pace of price increases is slowing.
Newly released video shows the husband of former U.S. House Speaker Nancy Pelosi fighting for control of a hammer with his assailant during a brutal attack in the couple’s San Francisco home last year.
The Biden administration released the "renters' bill of rights" as rent prices soar.
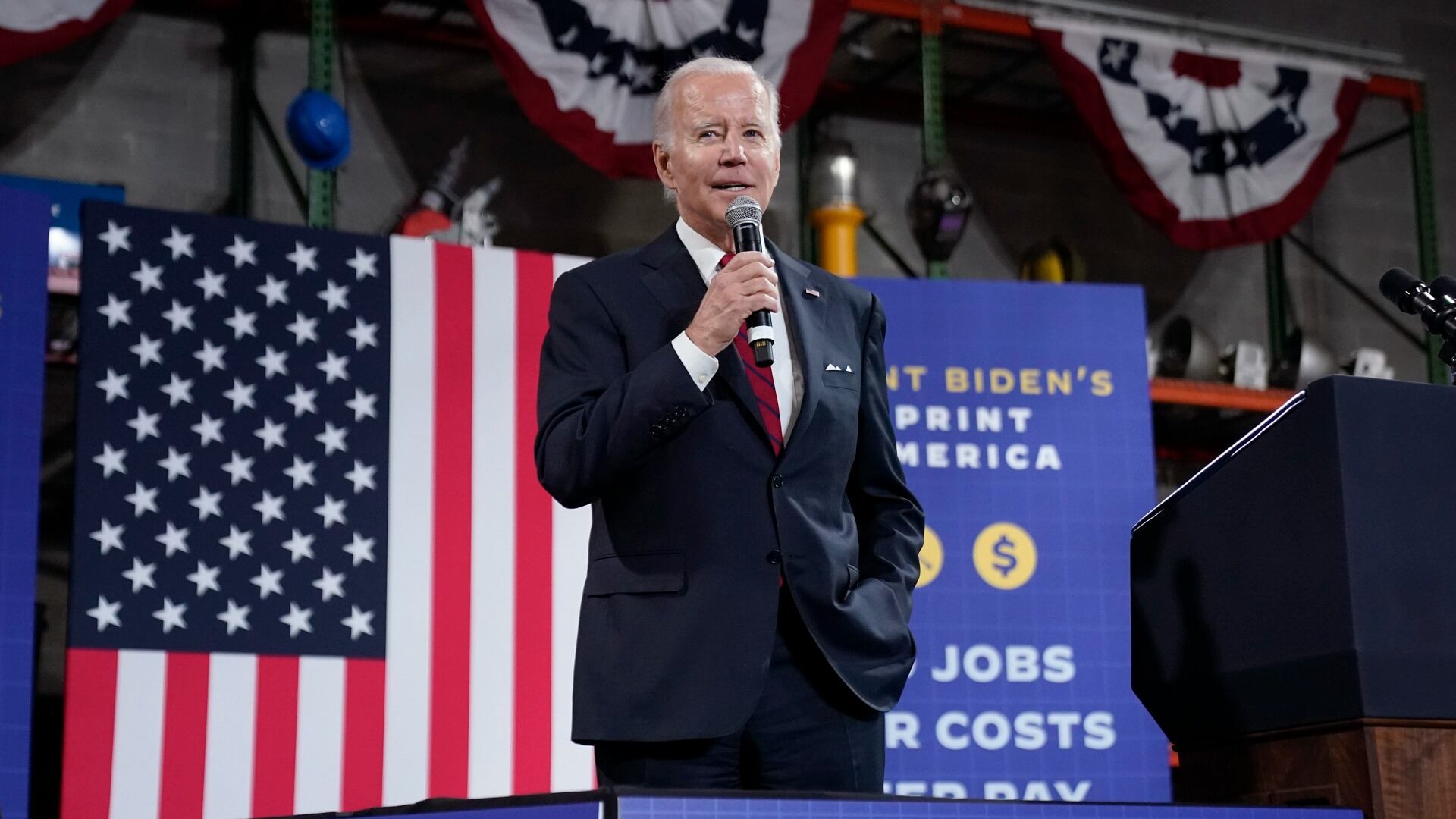
President Joe Biden touted the administration's economic achievements in a Virginia speech, while bashing Republicans for their handling of the nation's debt ceiling.